Andaman7 and Patient Participation: A Proven Approach to Filling Medication Data Gaps (JAMIA Open Study)
Accurate medication records are essential for safe and effective healthcare. Yet, as our recent study published in JAMIA Open shows, Electronic Health Records (EHRs) alone often fail to capture the full picture. Gaps are common, especially for over-the-counter (OTC) products, changes in medication usage, and adherence patterns.
This is where patients themselves can make a crucial difference. When equipped with the right tools, patients can record their medications with remarkable accuracy—our study showed an overall accuracy of 92%. By involving patients directly, we can fill the data gaps that EHRs and claims data often leave behind.
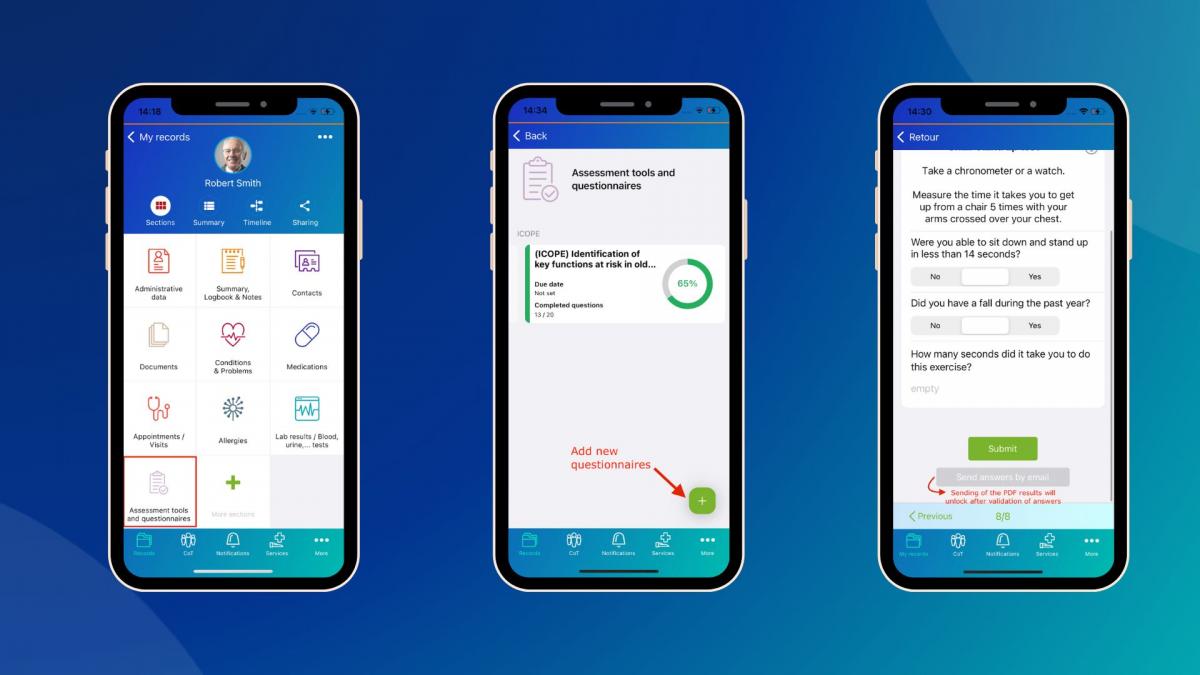
The Andaman7 platform empowers patients to take an active role in documenting their health. Its intuitive medication module supports multiple entry methods, including picklists, free text, and import from portals, allowing patients to record prescription and OTC medications, daily usage, and adherence. This patient-mediated approach aligns perfectly with the World Health Organization’s (WHO) concept of the “Best Possible Medication History” (BPMH).
Even beyond medications, Andaman7’s experience shows that patients can contribute valuable data on symptoms, daily health notes, and less acute conditions—information often missing from traditional records. With patients in the loop, records are more complete and accurate.
In short, patient-generated health data isn’t just a nice-to-have; it’s central to creating a complete, accurate, and actionable health record. Andaman7 makes that possible, bridging the gaps between what’s recorded in EHRs and what patients actually take every day.
For those interested in the full study, you can read the JAMIA Open publication here: https://www.andaman7.com/MyMMRJamniaArticle